Every year, the U.S. engages in a battle. The enemy trickles in when the leaves start to change, and doesn’t make the extent of its presence known until late winter. The soldiers never quite look the same, with modified weapons and a myriad of disguises. All summer, the good guys guess how to best defend their country. But, the same conditions of attack surface in the population year after year: the fever, sore throat, cough, muscle aches, and fatigue of the Influenza Virus. The guessing game, in terms of vaccine production, that scientists play impacts the severity of flu burden on the U.S. population. Comparing the 2017-2018 season (61,000 influenza-related deaths) with the 2018-2019 (34,200 influenza-related deaths) season displays the massive variability in disease incidence and mortality. The CDC has estimated 12,00 influenza-related deaths so far this season (2019-2020). Other contributing factors are overall national attitudes towards vaccines and knowledge of the threat of influenza.
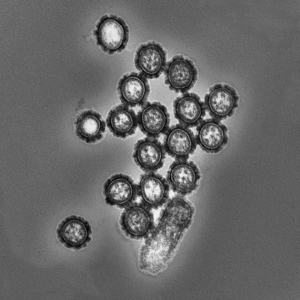
Depicted above is a generic flu virus, showing its enveloped structure and negative-sense, single-stranded RNA genome, segmented into either 7 (type C) or 8 (type A and B) pieces. Embedded in the envelope of type A and B are two distinct glycoprotein spikes, hemagluttinin antigen (HA) and neuraminidase antigen (NA). HA allows the virus to attach to host respiratory epithelium and NA is necessary for the production of new virions within a host. These factors, which are coded for by different genes in the virus’s segmented RNA, are variable, ever-mutating and responsible for the continuous spread of disease. Flu vaccines are made for type A and B viruses, with type A usually having more severe presentation. Initially more type B cases were observed this season, but the proportion of reported type A viruses is steadily increasing. Type A viruses are able to present in a range of species which increases their virulence. Whole RNA segments between species specific viruses are able to combine within an envelope and form an unrecognizable influenza variant, which is when pandemics (such as H1N1 in 2009) are usually observed.
All vaccines this season contain an updated version of hemagluttinin from the H1N1, H3N2, and 1-2 strains of type B viruses. The vaccine was 47% effective in the 2018-2019 season and is currently showing a range of 40-60% for this season. Despite reported effectiveness, receiving the vaccine confers some protection against all influenza infections even if the transmitted virus’s genome has mutated beyond the limits of the constructed vaccine. With the goal of preventing death tolls from climbing, it is important for all people to get the vaccine because even a slight immunological memory can decrease illness severity. Since children often have the highest attack rates of influenza virus, and are a key step in the widespread transmission of disease to households and at-risk communities, routine yearly vaccinations are especially encouraged. This survey uncovers some population wide misconceptions and excuses for not getting the flu vaccine. The most prevalent reasons include “forgetting” and not understanding the severity of the disease. It is not too late to receive the vaccine, participate in the yearly fight, and contribute to reducing influenza impact.